Chickenpox is a highly contagious illness caused by primary infection with varicella zoster virus (VZV). It generally begins with a vesicular skin rash appearing in two or three waves, mainly on the body and head rather than the hands and becoming itchy raw pockmarks, small open sores which heal mostly without scarring.
Chickenpox has a 10-21 day period and is spread easily through aerosolized droplets from the nasopharynx of ill individuals or through direct contact with secretions from the rash. Following primary infection there is usually lifelong protective immunity from further episodes of chickenpox.
Chickenpox is rarely fatal, although it is generally more severe in adults than in children. Pregnant women and those with a suppressed immune system are at highest risk of serious complications. The most common late complication of chicken pox is shingles, caused by reactivation of the varicella zoster virus decades after the initial episode of chickenpox.
Signs and symptoms
Chickenpox is a highly contagious disease that spreads from person to person by direct contact or by air from an infected person's coughing or sneezing. Touching the fluid from a chickenpox blister can also spread the disease. A person with chickenpox is contagious from one to five days before the rash appears. The contagious period continues until all blisters have formed scabs, which may take 5 to 10 days.[1] It takes from 10 to 20 days after contact with an infected person for someone to develop chickenpox.[2]
The chicken pox lesions (blisters) start as a two to four millimeter red papule which develops an irregular outline (a rose petal). A thin-walled, clear vesicle (dew drop) develops on top of the area of redness. This "dew drop on a rose petal" lesion is very characteristic of chickenpox. After about 8 to 12 hours the fluid in the vesicle becomes cloudy and the vesicle breaks leaving a crust. The fluid is highly contagious, but once the lesion crusts over, it is not considered contagious. The crust usually falls off after seven days sometimes leaving a crater-like scar. Although one lesion goes through this complete cycle in about seven days, another hallmark of chickenpox is that new lesions crop up every day for several days. Therefore it may be a week before new lesions stop appearing and existing lesions crust over. Children should not be sent back to school until all lesions have crusted over.[3]
It is not necessary to have physical contact with the infected person for the disease to spread. Infected persons can spread chickenpox before they know they have the disease, i.e. before any rash develops. They can infect others from about two days before the rash develops until all the sores have crusted over, usually four or five days after the rash starts.
Infection in pregnancy and neonates
Varicella infection in pregnant women can lead to viral transmission via the placenta and infection of the fetus. If infection occurs during the first 28 weeks of gestation, this can lead to fetal varicella syndrome (also known as congenital varicella syndrome). Effects on the fetus can range in severity from underdeveloped toes and fingers to severe anal and bladder malformation. Possible problems include:
Damage to brain: encephalitis, microcephaly, hydrocephaly, aplasia of brain
Damage to the eye (optic stalk, optic cap, and lens vesicles), microphthalmia, cataracts, chorioretinitis, optic atrophy
Other neurological disorder: damage to cervical and lumbosacral spinal cord, motor/sensory deficits, absent deep tendon reflexes, anisocoria/Horner's syndrome
Damage to body: hypoplasia of upper/lower extremities, anal and bladder sphincter dysfunction
Skin disorders: (cicatricial) skin lesions, hypopigmentation
Infection late in gestation or immediately following birth is referred to as neonatal varicella. Maternal infection is associated with premature delivery. The risk of the baby developing the disease is greatest following exposure to infection in the period 7 days prior to delivery and up to 7 days following the birth. The baby may also be exposed to the virus via infectious siblings or other contacts, but this is of less concern if the mother is immune. Newborns who develop symptoms are at a high risk of pneumonia and other serious complications of the disease. Path physiology
Chickenpox is usually acquired by the inhalation of airborne respiratory droplets from an infected host. The highly contagious nature of VZV explains the epidemics of chickenpox that spread through schools as one child who is infected quickly spreads the virus to many classmates. High viral titers are found in the characteristic vesicles of chickenpox; thus, viral transmission may also occur through direct contact with these vesicles, although the risk is lower.
After initial inhalation of contaminated respiratory droplets, the virus infects the mucosae of the upper respiratory tract. Viral proliferation occurs in regional lymph nodes of the upper respiratory tract 2-4 days after initial infection and is followed by primary viremia on postinfection days 4-6. A second round of viral replication occurs in the body's internal organs, most notably the liver and the spleen, followed by a secondary viremia 14-16 days postinfection. This secondary viremia is characterized by diffuse viral invasion of capillary endothelial cells and the epidermis. VZV infection of cells of the malpighian layer produces both intercellular and intracellular edema, resulting in the characteristic vesicle.
Exposure to VZV in a healthy child initiates the production of host immunoglobulin G (IgG), immunoglobulin M (IgM), and immunoglobulin A (IgA) antibodies; IgG antibodies persist for life and confer immunity. Cell-mediated immune responses are also important in limiting the scope and the duration of primary varicella infection. After primary infection, VZV is hypothesized to spread from mucosal and epidermal lesions to local sensory nerves. VZV then remains latent in the dorsal ganglion cells of the sensory nerves. Reactivation of VZV results in the clinically distinct syndrome of herpes zoster (shingles).
Diagnosis
Please help improve this section by expanding it. Further information might be found on the talk page. (March 2008)
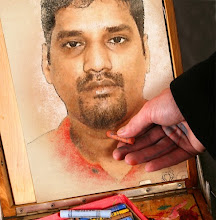
Early rash of smallpox vs chickenpox: rash mostly on the torso is characteristic of chickenpox
The diagnosis of varicella is primarily clinical. In a non-immunized individual with typical prodromal symptoms associated with the appropriate appearing rash occurring in "crops", no further investigation would normally be undertaken.
If further investigation is undertaken, confirmation of the diagnosis can be sought through either examination of the fluid within the vesicles, or by testing blood for evidence of an acute immunologic response. Vesicle fluid can be examined with a Tsanck smear, or better with examination for direct fluorescent antibody. The fluid can also be "cultured", whereby attempts are made to grow the virus from a fluid sample. Blood tests can be used to identify a response to acute infection (IgM) or previous infection and subsequent immunity (IgG).[5]
Prenatal diagnosis of fetal varicella infection can be performed using ultrasound, though a delay of 5 weeks following primary maternal infection is advised. A PCR (DNA) test of the mother's amniotic fluid can also be performed, though the risk of spontaneous abortion due to the amniocentesis procedure is higher than the risk of the baby developing foetal varicella syndrome.[4]
Prevention
A varicella vaccine was first developed by Michiaki Takahashi in 1974 derived from the Oka strain. It has been available in the U.S. since 1995 to inoculate against the disease. Some countries require the varicella vaccination or an exemption before entering elementary school. Protection is not lifelong and further vaccination is necessary five years after the initial immunization.[6]
In the United Kingdom, varicella antibodies are measured in women with no history of the disease as part of routine prenatal

No comments:
Post a Comment